Episode 12: Dr. Susan Scott – Nurse Scientist & Patient Safety Expert – The Second Victim Phenomenon, The Impact of Trauma on Clinicians, and Building Resiliency through Self-Care Systems
Summary
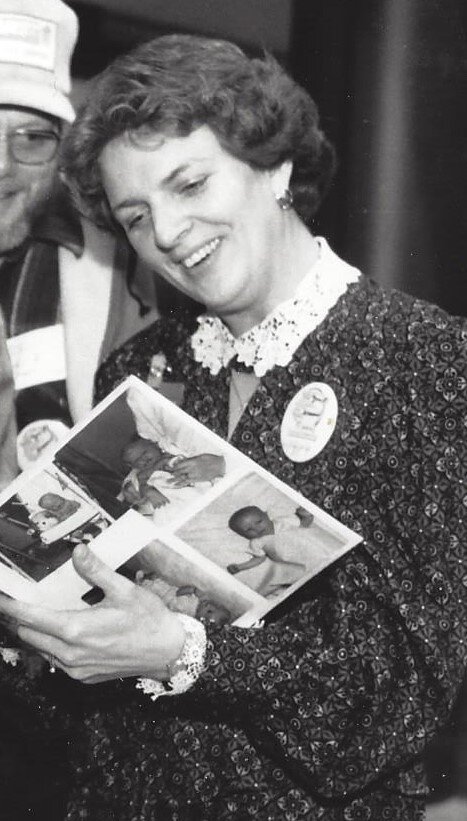
In this episode, our guest is Dr. Susan Scott, a nurse scientist and patient safety expert from University of Missouri Health Care.
Scott shares her research and personal experiences with the second victim phenomenon, the impact of trauma on a clinician’s work, strategies to support clinicians after traumatic events, and ways to combat burnout and low morale on a personal and institutional level.
Listeners will immediately connect to Scott’s passion as she describes her life’s work and its impact. Those inside and outside of healthcare will learn healthy ways to discuss and process trauma.
Show Notes
Understanding the Second Victim Phenomenon
Many healthcare studies are appropriately focused on patients, but Scott has spent decades studying an often-overlooked topic – clinicians who experience trauma from a medical error or unexpected outcome in their job known as the “Second Victim Phenomenon.” These traumatic events often come from the sudden death of a patient due to a medical error or unforeseen circumstances.
Scott shares the impact of these events on clinicians that most often lead to blame, isolation, and self-doubt. Many feel the need to ignore the trauma and “buck up and keep going” which only worsens its effects over time. Scott advocates for a dual-track intervention where institutions design support systems for both the patient’s family and the clinical care team of the patient.
Her studies have revealed three possible responses as a clinician tries to heal:
Thriving – Those that either already have a healthy support system to talk about the difficulties of their work or seek help from their institution or those focused on the subject, like Scott.
Survivors – The majority of second victims who show up to work but aren’t fully themselves or fully present because of the unresolved trauma. This is also known as presenteeism.
Dropouts – This is the response Scott focuses on most often, who at their best may change their careers and at their worst, end in suicide.
How Trauma Impacts Work
An important step in reaction to a second victim event is emotional first aid, which Scott found that only 15% of care providers will ask for help on their own. That leaves 85% of clinicians just trying to deal with it as they go about their clinical work. The simplest solution is implementing a peer support model that gives clinicians the space and structure to have these important conversations with colleagues instead of pretending like an event didn’t happen.
Scott explains that even though some may not think of these events as typical physical trauma cases, psychological trauma can be particularly dangerous because it goes unnoticed. This applies outside of a healthcare environment as well, as King and Scott consider the impact of small traumas over time in business. The pandemic has hopefully brought a greater awareness to the importance of empathy and caring for other humans in the difficult circumstances that life brings.
How Dr. Scott Developed a Passion for the Second Victim
Scott shares her own traumatic second victim experience just a few weeks into her first role as a newly graduated Registered Nurse, and the lack of tools she was given to process it. Even her mentor approached the event with a “welcome to nursing, don’t ever look back” attitude that left no room to have a conversation about the personal impact of that event.
As she advanced in her career and started as a Patient Safety Officer it become more apparent how pervasive the second victim suffering was and how ill-equipped providers were to deal with it. She never imagined her career moving in that direction, but the study of this phenomenon quickly became what she now describes as her life’s work.
The Role of a Patient Safety Officer
Before she became a Patient Safety Officer, Scott worked as a Legal Nurse Consultant helping defense teams look at medical records and support clinical staff. Although a short part of her career, it prepared her well for the patient safety roles and gave her the opportunity to advance the science while working at University of Missouri Health Care.
Scott describes how they’ve learned how to better address patient safety issues with providers by focusing on how they feel before charging in with education, compliance, and process improvements. From a patient safety standpoint, they seek to build systems that make error-prone humans as error-free as possible and pushing them toward the “thriving” response when incidents do happen.
Building Resiliency with Self-Care and Institutional Care
With nurse burnout and morale at a low point during the COVID-19 pandemic, Scott shares the importance of not just self-care practices but also the role of institutions caring for their employees. There are countless resources for self-care that deploy an “opt in” strategy that leaves the burdens on the clinician to seek out care.
But an “opt out” strategy could be more effective at combatting burnout. The systems that institutions put in place can either promote or discourage staff resiliency and care. She recommends three practices to incorporate in everyday systems: 1) a sense of belonging and community, 2) practicing gratitude, and 3) promoting positivity.
---
Closing
Humans in Healthcare is produced by Shearwater Health in Nashville, TN, and hosted by Chief Marketing Officer, Nathan King.